What Country Has the Worst Mental Health in the World?
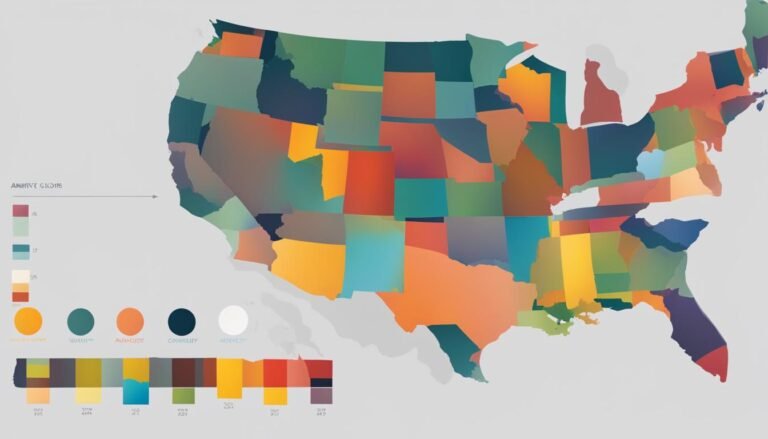
When it comes to mental health, some countries face more significant challenges than others. In a study comparing the mental health burden among high-income countries, it was found that the United States has one of the highest rates of mental health issues. With approximately one-quarter of U.S. adults reporting a mental health diagnosis or experiencing emotional distress, the country ranks among the worst in terms of mental health statistics.
Key Takeaways:
- The United States has one of the highest rates of mental health issues among high-income countries.
- About one-quarter of U.S. adults report a mental health diagnosis or experience emotional distress.
- The United States has the highest suicide rate and second-highest drug-related death rate among the countries studied.
- The U.S. has a lower supply of mental health workers compared to other countries, impacting access to care.
- Addressing the mental health crisis requires strategies such as integrating mental health care into primary care and expanding the mental health workforce.
Prevalence of Mental Health Conditions in the United States
In 2016, nearly one-quarter (23%) of U.S. adults reported having a mental health diagnosis, such as depression or anxiety, which is higher compared to other high-income countries. The incidence of mental health conditions may reflect differences in physician diagnostic patterns and cultural factors.
It’s important to note that not everyone who experiences mental health symptoms seeks professional help, so self-reports of emotional distress can provide a better understanding of the actual mental health burden. Approximately 26% of U.S. adults reported experiencing emotional distress in the past two years, similar to other countries like Canada and Sweden.
“The prevalence of mental health conditions in the United States is a significant concern. The high rates of mental health diagnoses and emotional distress highlight the need for effective mental health care and support systems.”
Understanding the prevalence of mental health conditions in the United States is crucial for developing strategies to address and mitigate the impact of these conditions on individuals and society.
The Importance of Mental Health Diagnosis Rates
The high mental health diagnosis rates in the United States indicate both a growing recognition of mental health issues and the need for appropriate support and treatment. With a significant portion of the population experiencing mental health conditions, it is essential to prioritize mental health care and destigmatize seeking help.
Emotional Distress and its Implications
Emotional distress, which encompasses a range of psychological symptoms and challenges, is also prevalent in the United States. These symptoms can have a significant impact on an individual’s well-being, functioning, and overall quality of life, warranting the provision of accessible and effective mental health services.
By acknowledging the prevalence of mental health conditions and emotional distress in the United States, policymakers, healthcare providers, and society at large can work towards implementing strategies that promote mental health awareness, access to care, and the overall well-being of individuals affected by these conditions.
Factors Contributing to Mental Health Issues in the U.S.
Social and economic factors play a significant role in the high prevalence of mental health issues in the United States. A study found that nearly half (45%) of U.S. adults experiencing emotional distress also reported concerns about neighborhood safety or having enough money for housing or food. These social and economic challenges contribute to unmet social needs, potentially increasing the likelihood of experiencing emotional distress.
Cultural norms and stigma surrounding psychological illness also impact mental health disparities in the U.S. In comparison to some other countries, there is less stigma associated with seeking treatment for mental health concerns. This more accepting cultural attitude may positively influence individuals’ likelihood of seeking mental health care, leading to better outcomes.
“Social and economic factors contribute to unmet social needs, potentially increasing the likelihood of experiencing emotional distress.”
Addressing social and economic factors, along with reducing stigma, is crucial in improving mental health outcomes in the United States. By implementing policies and interventions that address housing security, income disparities, and neighborhood safety, the U.S. can create healthier environments that support mental well-being.

Access and Affordability of Mental Health Care in the U.S.
Access to mental health care and affordability are significant barriers in the United States, hindering individuals from receiving the help they need. While U.S. adults exhibit a strong willingness to seek professional assistance for emotional distress, they also encounter notable challenges when it comes to accessing and affording mental health care services.
According to a recent study, approximately 15% of U.S. adults who have experienced emotional distress in the past two years reported being unable to obtain or afford professional help. This highlights the pervasive barriers that individuals face when attempting to access the necessary mental health care resources.
These access and affordability issues contribute to the high suicide rate in the U.S., which surpasses that of the 11 countries included in the study. Comparatively, even though France also experiences a high suicide rate, the U.S. rate is nearly double that of the country with the lowest number of suicides, the U.K.
The Impact of Barriers to Accessing Mental Health Care
The inability to access and afford mental health care can have severe consequences for individuals and society as a whole. Without proper care, individuals may struggle to manage their mental health conditions, leading to worsening symptoms, decreased quality of life, and potential harm to themselves or others.
“Access and affordability are key factors that determine whether individuals with mental health issues are able to receive the necessary treatment and support. When these barriers exist, it perpetuates a cycle of unmet needs and worsening outcomes.”
Hence, addressing these barriers is crucial to improve mental health outcomes and reduce the overall burden of mental illness.
The Need for Solutions
To overcome the challenges related to accessing and affording mental health care, it is crucial to implement targeted solutions that enhance accessibility and affordability. This includes:
- Expanding mental health care coverage and reducing out-of-pocket costs for mental health services.
- Increasing the number of mental health care providers and ensuring their distribution is equitable.
- Integrating mental health care into primary care settings to improve access and reduce stigma.
- Implementing telehealth services to widen access to mental health care, particularly in underserved areas.
- Providing comprehensive mental health education and awareness programs to reduce the stigma associated with seeking help.
By addressing the access and affordability barriers, the U.S. can work towards building a more inclusive and effective mental health care system that meets the needs of all individuals.
Mental Health Workforce and Capacity in the U.S.
The United States faces challenges when it comes to the mental health workforce and its capacity to meet the mental health needs of its population. Compared to other high-income countries, the U.S. has a relatively low supply of mental health workers, which impacts the accessibility of mental health care.
Currently, there are only 105 mental health professionals per 100,000 people in the United States, lagging behind countries like Canada, Switzerland, and Australia, which have approximately twice that number of mental health workers. This shortage negatively affects the ability to provide timely and comprehensive care to those in need.
In the U.S., the mental health workforce mainly consists of social workers and nurses, while the supply of psychologists and psychiatrists is lower compared to most other countries. This limited number of mental health professionals specialized in psychology and psychiatry further exacerbates the strain on the mental health workforce.
Furthermore, only one-third of primary care practices in the U.S. have a mental health provider on their patient care teams. This statistic highlights the limited capacity of the U.S. health system to adequately address mental health needs. The integration of mental health professionals into primary care settings is crucial for early intervention and comprehensive treatment.

To strengthen the mental health workforce and capacity in the U.S., concerted efforts are required. This includes increasing the recruitment and training of mental health professionals, particularly psychologists and psychiatrists. Additionally, prioritizing the integration of mental health care into primary care settings can improve access to services and enhance the overall continuity of care.
In conclusion, the United States needs to address the shortage of mental health workers and enhance its capacity to meet the mental health needs of its population. By investing in the mental health workforce and integrating mental health care into primary care settings, the U.S. can take significant steps toward providing comprehensive and accessible mental health services to its citizens.
Conclusion
The United States is confronted with significant mental health challenges, grappling with one of the highest mental health burdens among high-income countries. A combination of factors, including social and economic needs, access and affordability issues, and a constrained mental health workforce, contribute to the poor mental health outcomes in the nation. To combat the global mental health crisis and address mental health disparities across countries, it is essential to draw inspiration from the strategies implemented by other high-income nations.
One effective strategy is the integration of mental health care into primary care settings. By embedding mental health services within primary care, individuals can access comprehensive care that addresses both physical and mental health needs. This approach has been successful in countries like Canada, Switzerland, and Australia, allowing for more coordinated and accessible mental health services.
In addition, removing cost-related access barriers is crucial. High treatment costs often deter individuals from seeking the necessary care, exacerbating the mental health crisis. Following the example of countries like Sweden, where mental health care is heavily subsidized or offered at low or no cost, can improve affordability and increase mental health service utilization rates.
Furthermore, expanding the mental health workforce is essential for strengthening mental health care in the United States. Countries with a higher supply of mental health workers, such as Canada and Switzerland, tend to experience better mental health outcomes. Increasing the number of psychologists, psychiatrists, and other mental health professionals, while also ensuring their equitable distribution across regions, is crucial for meeting the growing mental health needs of the population.
Addressing the global mental health crisis requires a comprehensive and coordinated effort. By implementing strategies that have proven successful in other high-income nations, such as integrating mental health care into primary care, removing cost-related access barriers, and expanding the mental health workforce, the United States can make significant strides in improving overall well-being and reducing the impact of mental health issues on individuals and society.
FAQ
What country has the worst mental health in the world?
According to a study comparing the mental health burden among high-income countries, the United States has one of the highest rates of mental health issues.
What are the prevalence rates of mental health conditions in the United States?
In 2016, nearly one-quarter of U.S. adults reported having a mental health diagnosis, such as depression or anxiety, which is higher compared to other high-income countries.
What factors contribute to mental health issues in the U.S.?
Social and economic factors, such as concerns about neighborhood safety and financial instability, contribute to the high prevalence of mental health issues in the United States.
What are the barriers to accessing mental health care in the U.S.?
Access and affordability issues are significant barriers to mental health care in the United States, with a significant percentage of adults reporting difficulties in getting or affording professional help.
What is the mental health workforce and capacity like in the U.S.?
The United States has a relatively low supply of mental health workers compared to other high-income countries, with a limited capacity to meet the mental health needs of the population.
What needs to be done to address the global mental health crisis?
To address the global mental health crisis and reduce disparities across countries, strategies such as integrating mental health care into primary care and expanding the mental health workforce need to be implemented.
Source Links
- https://www.commonwealthfund.org/publications/issue-briefs/2020/may/mental-health-conditions-substance-use-comparing-us-other-countries
- https://worldpopulationreview.com/country-rankings/depression-rates-by-country
- https://www.usnews.com/news/best-countries/slideshows/the-most-depressed-countries-in-the-world